What is a TBI?
Traumatic Brain Injury (TBI) is the broad term used to describe an injury to the brain that is not intrinsic to a person from birth. While brain hemorrhages and stroke caused by a brain clot are considered a form of TBI, this medical term is more commonly used to describe an acquired brain injury caused by a blow or jolt to the head (1). In addition, a TBI itself can increase the risk of having a stroke or brain hemorrhage and thus experiencing detrimental physical effects on motor skills, speech and cognition.
Since car or motorcycle accidents, sports injuries, and “slip and fall” accidents are all linked to an increased risk of TBI, an understanding of the symptoms, severity, assessment methods, treatments, and differences between the most common forms is essential. These are described in this article to assist TBI survivors in boosting their chances of recovery.
What is a TBI and How is it Diagnosed?
In the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5), TBI is defined as brain trauma with specific characteristics that include at least one of the following (2):
- Loss of consciousness
- Post-traumatic amnesia (complete memory loss of event)
- Disorientation and confusion
- In severe cases, neurological signs such as onset of recurrent seizures, loss of sense of smell/taste, or a narrowing of visual field
Since persistent depressed mood often occurs following a moderate-to-severe TBI, an accurate diagnosis is crucial to accessing mental health services after experiencing a TBI. More than 450,000 US military service members were diagnosed with a TBI between 2000-2021, and many have since been co-diagnosed with clinical depression or PTSD (3).
Neurological assessments for TBI include CT scans and MRI scans, but they are often unable to reveal evidence of mild TBI and thus are not used to diagnose concussions. The neurological exam used in assessing TBI severity evaluates motor function/movement, sensory function, thinking ability, normal eye movement, and normal reflexes (4). The assessments used for diagnosing TBI existence and severity are also used by outpatient physicians and physical therapists to demonstrate recovery progress over time.
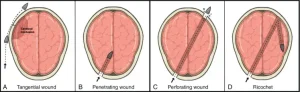
Understanding TBI – Types and Levels as Linked to TBI Symptoms and Prognosis
An acquired brain injury – not hereditary, congenital, degenerative, or caused by birth trauma – is categorized as either traumatic and non-traumatic (change this sentence); externally-caused brain injuries are categorized as traumatic, while other medical emergencies such as a stroke are considered non-traumatic (5). Currently, a brain injury must be acquired to receive a diagnostic code of TBI by a medical clinician which includes a diagnostic classification of mild, moderate, or severe. During the physician diagnostic exam, the TBI is also classified as penetrating or non-penetrating (6). Penetrating TBI is usually caused by a sharp object that pierces the skull, while a non-penetrating TBI can be caused by a slam of the head against another person’s head, ground or other object, persistent violent shaking, or by blast waves resulting from an explosion.
https://www.sciencedirect.com/science/article/abs/pii/B9780323653855000135
The symptoms experienced depend largely upon the type and severity of the TBI, as well as whether the TBI is the first occurrence or repeating. A concussion is a very common type of TBI, and usually associated with a slam or bump to the head resulting in an injury that can range from mild to severe. Symptoms of a TBI, including a concussion, can be temporary or permanent.
Early concussion symptoms are any or all of the following (7):
- Headache
- Light sensitivity (photophobia)
- Nausea or dizziness
- Decreased ability to maintain attention or concentrate
- Problems with balance and/or coordination
Symptoms such as these can be delayed following the concussion for hours or even days. If the concussion is one that is moderate-to-severe, loss of consciousness and other more debilitating neurological symptoms can develop.
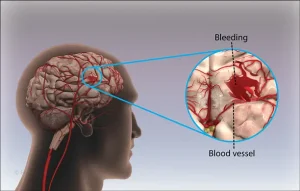
The more that the brain becomes inflamed as a consequence of the TBI, the greater the risk of experiencing a brain bleed. When the capillaries, veins, or arteries leak blood into the brain tissue, damage typically occurs that can affect nerve signaling to other parts of the body as well as cognitive abilities.
https://www.msn.com/en-za/health/condition/intracerebral-hemorrhage/hp-Intracerebral%20Hemorrhage
Depending upon where the bleeding occurs, the ability of a person to speak, understand language, and be able to move the extremities can be impacted. For this reason, assessing the severity of the TBI is crucial to understanding the proper treatment approach.
Penetrating TBIs, such as the result of a bullet or knife wound, are typically the most immediately severe in their symptoms and requirement for medical treatment. Generally, the severity of TBI-induced brain damage is linked to the need for and amount of physical therapy and the prognosis for recovery of lost motor, language, and cognitive skills.
According to the American Association of Neurological Surgeons, the most common symptoms following any type of TBI are (8):
- Pain (such as a continuous or recurring headache)
- Motor dysfunction (such as paralysis, weakness or involuntary shaking of the hand or fingers)
- Sensory changes (such as dizziness or change in sense of taste/smell)
- Cognitive changes (such as shortened attention span and a feeling of overstimulation by environmental sensory stimuli such as sounds)
- Speech problems (such as difficulty remembering/saying words and jumbled speech)
What is CTE?
Chronic Traumatic Encephalopathy (CTE) is a degenerative brain disorder associated with multiple occurrences of TBI. It is particularly found in military service members who served in armed conflict areas and football players or boxers, but can only be currently diagnosed upon autopsy after death. Multiple incidents of head trauma over a lifetime – such as multiple concussions – have been linked to CTE. The CTE occurrence causes changes over time in brain cells, and symptoms do not usually appear for years following the TBI injuries. Depression, uncontrolled outbursts of anger, and premature dementia are all symptomatic of CTE in people with a past history of multiple TBIs (9).
Comparison of Rehab Needs between Stroke and TBI Survivors
There is a tremendous overlap in the rehabilitation needs of stroke and TBI survivors. Physical and/or occupational therapy are both typically prescribed following either a stroke or TBI. Since TBI most often occurs with heightened frequency in a younger age demographic as compared to stroke, physical and occupational therapy activities need to be adjusted to align with patient age.
Additionally, due to the younger age demographic typically impacted by TBIs, physical and/or occupational therapy is often more intensively targeted toward full recovery in these patients – and even beyond the pre-TBI level of muscle strength. It is important to recognize that the senior-aged stroke survivor population often has other preexisting health issues such as joint osteoarthritis and cardiovascular disease that impact the ability to perform prescribed physical and occupational therapy regimens. Stroke-caused cognitive impairments may also be more difficult for senior-aged people to overcome.
Cognitive, Physical, and Psychological Symptoms of a TBI and Impact on Treatment
Though there are shared complications and symptoms when comparing strokes and traumatic brain injuries (TBIs), it’s crucial to bear in mind that a stroke is categorized as a non-traumatic brain injury.
Similar to stroke, a persistent cognitive deficit can occur following a TBI. In both stroke and TBI victims, the neurological signals in the brain that enable people to process new information, follow instructions, problem-solve, exert self-control over emotions, and access/store memories can become impaired. Neurologically-based depression and anxiety are common in people who have experienced a stroke or a TBI. The loss of motor skills such as walking and self-feeding can make stroke and TBI survivors feel hopeless about a return to independent functioning and disinclined to participate in physical or occupational therapy.
Professional, college, and high school athletes who are TBI survivors can also experience a profound and sudden change in their normal lives if they are no longer able to participate in the sport they loved. Likewise, military personnel can find themselves unable to continue pursuing their active duty goals and must endure separation from their colleagues. This can place an added stress on coping with recovering from a TBI.
Diagnosis and Treatment of Severe TBI
The type and severity of a TBI can necessitate a lengthy hospitalization stay and intense level of inpatient care. A skull fracture or the need to remove part of the skull to alleviate brain swelling can require skull surgeries. Paralysis of the lower extremities and/or incontinence due to disrupted spinal cord signaling to the bladder or bowels can call for a transfer to a rehab facility for several months prior to returning home. A prolonged period of being bed-bound can result in muscle-wasting in the unused extremities, as well as in spatial-temporal disorientation, loss of postural control, and lowered overall cognitive status (10). Therefore, progression from a bedbound status to a chair or better is an important patient care goal in TBI medical treatment.
Is a Stroke a TBI?
Stroke is considered different from a TBI, but TBI survivors are considered at increased risk of stroke compared to the general adult population. That increased stroke risk level is largely dependent on the severity of the TBI and whether or not it was a repeat TBI. However, the risk for Transient Ischemic Attacks (TIAs), popularly-called “mini-strokes”, is significantly increased for TBI survivors. People having a TIA may lose conscious awareness of their location or what they are doing for just a second, thus not realize a TIA has occurred and therefore may not seek care from a doctor. The issue lies in the fact that TIAs exponentially increase the risk for experiencing a stroke; therefore, for TBI survivors, it is imperative to recognize stroke symptoms and seek immediate medical assistance.
Comparing TBI and Stroke
Strokes are caused by a blockage in the blood flow to the brain, either by a blood clot or sudden bleeding. Clot-caused (ischemic) strokes are the most common and usually occur in senior-aged or middle-aged people with a history of poorly-managed diabetes (11). Hemorrhagic strokes are most often caused by a bulged artery (or vein) that has burst, such as from a TBI, and correspond to a higher likelihood of severe brain damage and rapid fatal outcome. Hemorrhagic strokes also include those caused by congenital venous aneurysms, which are often fatal.
In ischemic strokes, the carotid arteries that carry blood from the heart to the brain can become clogged by plaque build-up, resulting in one or more blood clots and death of nearby brain cells. Depending upon the location of the brain cell death, symptoms can include extremity paralysis and weakness, usually in the opposite side of the body from the brain hemisphere where the stroke occurred. While strokes on the right side of the brain typically are associated with limb paralysis, strokes on the left side of the body are typically associated with both limb paralysis and speech/language impairments.
Unlike with stroke, a TBI can cause swelling in the brain that can lead to pressure against the skull. In turn, that pressure can cause bleeding from the pressed blood vessels. If the skull is fractured due to accident or injury, a bone fragment can also cause bleeding. Whatever the cause of bleeding inside the brain, the result is the death of brain cells. Concussion can result in bruising rather than bleeding, which is why a concussion is diagnosed through a different clinical approach than other TBIs.
Conclusion
Whether a stroke or Traumatic Brain Injury (TBI), neurological damage can occur as linked to the severity of the brain injury. TBIs are caused primarily by external damage to the brain such as a blow or jolt to the head. In contrast, strokes are caused by blood clots and internal hemorrhage in the brain. However, a TBI places a person at significant risk for a future stroke. The severity of the stroke or TBI is highly-linked to the symptoms experienced, and both of these brain injuries can result in paralysis or weakness in the limbs. Nerve impulses from the brain that travel to the spinal cord transmit biochemical “messages” to the muscles, but can become impaired as a consequence of a stroke or TBI. That impairment can result in a loss of motor skills in the afflicted person, such as the ability to utilize arms, wrists, hands, and fingers in movements to accomplish routine activities of daily living.
If you have experienced a TBI and PT and/or OT has been prescribed for you, it is important that you adhere to the prescribed regimen and diligently perform your daily exercises. While you may initially experience difficulties, frustration and even feelings of hopelessness, remember that recovery to some degree is possible with effort and determination. In addition, being mindful of your risk level for stroke following TBI and being aware of its symptoms will help you to minimize the chance of further impairment. For more information on symptoms, treatment, and support, visit our resources page.
References:
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on the Review of the Department of Veterans Affairs Examinations for Traumatic Brain Injury. (April 10, 2019). B. Definitions of Traumatic Brain Injury. In: Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans. National Academies Press: Washington, DC. Webpage: https://www.ncbi.nlm.nih.gov/books/NBK542588/#:~:text=Traumatic%20brain%20injury%20(TBI)%2C,skull%20and%20enters%20brain%20tissue.
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on the Review of the Department of Veterans Affairs Examinations for Traumatic Brain Injury. (April 10, 2019). B. Definitions of Traumatic Brain Injury. In: Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans. National Academies Press: Washington, DC. Webpage: https://www.ncbi.nlm.nih.gov/books/NBK542588/#:~:text=Traumatic%20brain%20injury%20(TBI)%2C,skull%20and%20enters%20brain%20tissue.
- Centers for Disease Control (CDC). Traumatic Brain Injury & Concussion. TBI Among Service Members and Veterans. Webpage: https://www.cdc.gov/traumatic-brain-injury/health-equity/index.html
- US Food and Drug Administration (FDA). Traumatic Brain Injury: What to Know About Symptoms, Diagnosis, and Treatment. Webpage: https://www.fda.gov/consumers/consumer-updates/traumatic-brain-injury-what-know-about-symptoms-diagnosis-and-treatment#:~:text=Diagnosis%20of%20TBI&text=Assessment%20usually%20includes%20a%20neurological,scans%2C%20cannot%20detect%20all%20TBIs.
- Brain Injury Association of America (BIA). What is the difference between an acquired brain injury and a traumatic brain injury? Webpage: https://www.biausa.org/brain-injury/about-brain-injury/nbiic/what-is-the-difference-between-an-acquired-brain-injury-and-a-traumatic-brain-injury
- National Institute of Neurological Disorders and Stroke (NINDS). Traumatic Brain Injury (TBI). Webpage: https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi
- Mayo Clinic. Concussion. Webpage: https://www.mayoclinic.org/diseases-conditions/concussion/symptoms-causes/syc-20355594
- American Association of Neurological Surgeons (AANS). Concussion. Webpage: https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Concussion
- Concussion Legacy Foundation. Resource Center – What is CTE? Webpage: https://concussionfoundation.org/CTE-resources/what-is-CTE
- Cardoso R, Parola V, Neves H, et al. (2022). Physical Rehabilitation Programs for Bedridden Patients with Prolonged Immobility: A Scoping Review. International Journal of Environmental Research and Public Health 19(11): 6420. Webpage: https://www.mdpi.com/1660-4601/19/11/6420
- Centers for Disease Control (CDC). Stroke Facts. Webpage: https://www.cdc.gov/stroke/facts.htm#:~:text=About%2087%25%20of%20all%20strokes,to%20the%20brain%20is%20blocked.&text=Stroke%2Drelated%20costs%20in%20the,billion%20between%202018%20and%202019.